Attention A T users. To access the menus on this page please perform the following steps.
1. Please switch auto forms mode to off.
2. Hit enter to expand a main menu option (Health, Benefits, etc).
3. To enter and activate the submenu links, hit the down arrow.
You will now be able to tab or arrow up or down through the submenu options to access/activate the submenu links.
Locator
Contact
Search
VA »
Health Care »
VHA National Center for Patient Safety
»
NCPS APPROACH TO ACHIEVING HIGH RELIABILITY
VHA National Center for Patient Safety
NCPS APPROACH TO ACHIEVING HIGH RELIABILITY
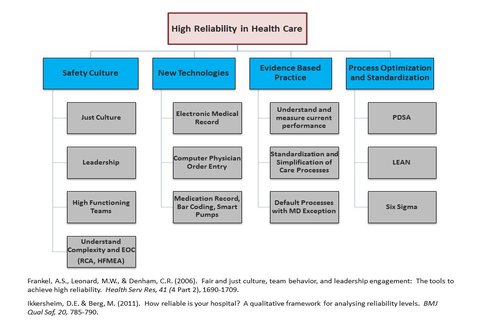
High Reliability in Health Care Diagram
Tuesday, October 11, 2016
To Create Highly Reliable Organizations (HRO) – Create a Safety CultureThe remarkable improvements seen in the U.S. aviation system have attracted the attention of the health care industry, which seeks to adopt some of its strategies for improving care. One important strategy pursued by the VA National Center for Patient Safety (NCPS) since its founding is high reliability science, or the study of organizations in high-risk industries that operate in safety sensitive settings while maintaining high levels of safety. Although High Reliability Organizations (HROs) have ample opportunity to fail, they have come to function in a manner that makes failures extremely rare. Members within such organizations structure their work toward the identification of failures. This results in the early identification of errors and error-producing processes. Weick and Sutcliffe (2007, 2015) have argued that HROs promote a manner of “organizational mindfulness” where all members watch for and report safety concerns before they pose risks to the larger organization.
The best performing HROs understand that disasters in complex sociotechnical systems are a result of multiple, small, and separate events that become intertwined and then amplified—ultimately allowing systems to “drift” into disaster. Regardless of the industry, those that have achieved the status of HRO share common features that are built upon intentional actions and ideas. Over time, these features define the “culture” (i.e. “the way things are done around here”) of these organizations—cultures that focus on safety. The challenge remains in how to translate the lessons articulated by Weick and Sutcliffe into a conceptual model that may yield for Veteran’s health care the successes enjoyed by other highly reliable industries.
For health care organizations, the term safety culture describes the contexts in which patient care is delivered as well as the shared values, attitudes and behaviors that determine how organizational members minimize patient harm during the delivery of care. A culture of safety has several elements: just culture, engaged leadership, high- functioning clinical teams, perpetual training cycles and an understanding of complexity that includes robust process improvement practices. These elements alone will not establish high reliability, but are an essential first step.
Just Culture:
A Just Culture recognizes that even the most committed professionals will make mistakes and that unhealthy behaviors, such as short cuts and workarounds, are common in the face of pressures to maximize efficiency. However, there is no tolerance in a Just Culture for behaviors that repeatedly or purposefully violate steps put in place to maintain safety. Thus, both accountability and appropriate psychological safety are balanced. When a close call, or adverse event occurs, a Just Culture is focused on the “why” not the “who.”
Assuming that no one comes to work with purposeful intent to harm patients, it is important for organizations in the wake of adverse events to move beyond the blame and shame approach, which encourages workers to hide mistakes, and instead facilitate the thoughtful detection of imbedded system vulnerabilities that contribute to patient harm.
Engaged Leadership:
Individuals in top leadership positions are the driving force behind how things function in a health system and are absolutely essential to creating a safe culture. It is critical for leadership to make safety part of the daily discussion and a center point of major meetings and strategy sessions. Top leaders must also craft a reporting relationship that ensures safety officers deliver unfiltered information to key decision makers in the organization.
High Functioning Clinical Teams:
Health care is provided by interdependent teams of medical professionals who should share a common goal toward delivery of Veteran care. To create such an environment, the members of the team must have a shared mental model that allows each person to maintain situational awareness regarding progress toward that shared goal.
Situational awareness is the continuous perception of team functioning in relation to a constantly changing environment, including the ability to make changes as appropriate to an evolving situation. It includes awareness of critical information, comprehending the true meaning of this information, communicating that information and planning for future possibilities. High-functioning teams are well versed on leader strategies to foster participation so that all team members embrace the responsibility to speak up about perceived risks in the operational setting. Likewise team members regularly implement standardized methodologies for practicing assertive inquiry and advocacy to preserve safety when necessary.
Perpetual Training Cycles:
A hallmark of any high reliability industry is a steadfast commitment to perpetual training – both in the technical and non-technical elements of the job (such as competency in teamwork, communication and situational awareness). For example, the training signature in commercial aviation includes initial training followed by a series of recurrent training experiences at specified intervals that continue indefinitely for one’s professional life cycle. This training includes both team and individual practice followed by competence evaluation under observation using high-fidelity simulation. For health care to approach high reliability, it must – at a minimum – move away from single episode training toward a training signature where multidisciplinary teams train together on a perpetual basis.
Understanding Complexity:
Health care systems are complex: They consist of a multitude of interdependent and diverse components that adapt to changes in the environment. Because the components of the health care system will interact and adapt as change is introduced, it is imperative that a culture values the reporting of errors, concerns, risks or near misses in order for it to prevent or mitigate potential harms. The only way to identify emerging vulnerabilities is to develop an organizational culture that is willing to bring up, discuss, and address its problems. This is why a Just Culture is such a critical part of any complex system. To have any hope of catching vulnerabilities before they cause harm, we must have vigilant staff continuously scanning for minor vulnerabilities that may conspire to result in major accidents. Those staff must be armed both with the tools to deeply understand the evolution of harm through the care delivery system, as well as the ability to analyze and improve their own work environment. Critical to accomplishing this objective is a leadership that is receptive to staff feedback regarding errors, concerns and near misses.
Improving Processes:
Successful integration of quality improvement strategies within health care settings require organizations to meet a number of well-defined challenges, including the complexity of human disease and the dynamic nature of safety. Chief among these hurdles is the inability of a narrow “tools and methods approach” to institutionalize quality improvement. For example, most organizations never make it past thinking of Lean as a series of “tools” that can improve the system. Unfortunately, the best tools will fail to yield lasting improvements if the existing culture upon which the tools are dispersed is lacking the rudiments of a safe and transparent culture. Process improvement efforts must also be communicated in concert with continuous efforts to create, nurture, and sustain a foundationally safe culture. In this way, VA utilizes Lean as a standardized methodology for how process improvement is approached.
To develop a health care organization where staff freely and respectfully challenge supervisors when safety is in question, a trust must be cultivated that communicates to staff that they will not be penalized for doing so. A major goal of the health care industry today is to morph from a culture that sees errors as ‘weakness, laziness, or lack of commitment’ subject to punishment, to one where errors are seen as an inevitable consequence of the limits of human performance. In the latter, errors are freely voiced as part of a just culture: They are discussed as teachable moments for learning more about prevention and management. Team members are therefore encouraged to not only follow standard procedures, but also contribute to problem-solving via prompt intervention when preventable errors and harms are anticipated.
The programs of NCPS in partnership with many other entities and people across VHA are working to make care safer, with an eye toward consistent improvement. The diagram above is a conceptual framework for achieving high reliability – while achieving a culture of safety is critical, many additional efforts are needed.



















