Decreasing preventable VTE outcomes
Decreasing preventable VTE outcomes (Figure 1.)
Documented secondary assessment decreases preventable VTE outcomes
Jennifer L. Cole, Pharm.D., BCPS, BCCCP, clinical pharmacist, Veterans Healthcare System of the OzarksBackground:
Venous thromboembolism (VTE) continues to be a major cause of morbidity and mortality with approximately 100,000 confirmed deaths annually in the United States.1 Efforts to improve the implementation gap for VTE prophylaxis guidelines into practice have been ongoing for decades. In 2008, the VA Office of Inspector General (OIG) evaluated adherence to evidence-based recommendations for prevention of VTE in hospitalized patients. The Prevention of VTE in VA Hospitals Report (06-02459-209) estimated that only 63% of at-risk patients received appropriate VTE prophylaxis.
The OIG recommends all VA facilities to develop and implement a plan to ensure appropriate VTE preventative therapies for at-risk hospitalized patients. In 2014, the VA OIG investigated potentially preventable pulmonary embolisms (PE) at 29 VHA medical facilities. The Preventable PE at VA Facilities Report (14-01073-139) revealed that 15% of 259 confirmed PEs with at least one PE risk factor had missed or delayed PE diagnosis or inadequate prophylaxis.
The Veterans Healthcare System of the Ozarks (VHSO) initially adopted a VTE prevention program in 2009 utilizing a “Three Bucket” model to stratify patients into low, moderate, or high risk groups based on known VTE risk factors.2 Providers were required to evaluate hospitalized patients via computerized checklist within 24 hours of admission or transfer.
In 2013, a VTE related adverse event at the facility led to a Root Cause Analysis. A multidisciplinary task force was challenged with creating a strategy to augment existing VTE prevention efforts. They found that the inpatient clinical pharmacist was in a unique position to evaluate admitted patients for appropriate pharmacologic prophylaxis.
Methods:
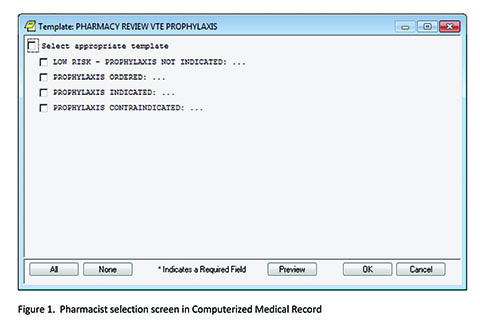
A new CPRS note title and template were developed: Pharmacy Review VTE Prophylaxis (Figure 1). The template has four selections: 1) low risk, 2) prophylaxis ordered, 3) prophylaxis indicated, and 4) pharmacologic prophylaxis contraindicated. The selection options had prefilled text that could be modified, if needed. If option three (prophylaxis indicated) was selected, the patient’s provider was added to the note for co-signature. These notes were stored in the progress notes of the patient’s permanent medical record. The VTE prevention effort was further enhanced with reminders of VTE prophylaxis embedded in the nursing shift assessment.
The novel note and template went into effect in January 2014. All hospitalized patients should have the assessment and note completed in CPRS within 48 hours of admission. The facility set a benchmark of 90% for this quality initiative.
Results:
Inpatient VTE complications were later compared in before and after cohorts. Over 36,000 discharges were reviewed between 2008 to 2018 for incidence of VTE events before and after the 2014 pharmacy intervention. Aggregate data from VA’s Strategic Analytics for Improvement and Learning (SAIL) were reviewed for inpatient VTE events and 30-day readmissions for VTE. The augmented assessment strategy led to a decrease in both inpatient VTE (0.20% to 0.11%), and 30-day readmissions for VTE (0.16% to 0.04%).
Rates of appropriate prophylaxis were studied after the 2014 intervention through VA Inpatient Evaluation Center (IPEC) monitoring. The combined pharmacologic prophylaxis rate was 86% with 92% present in high-risk ICU patients and 81% in acute care patients.
Discussion:
VTE reduction strategies should be multi-faceted for best outcomes, such as electronic decision support which is supplemented with prospective audit and feedback. VTE risk factors should be assessed frequently during an inpatient stay because a change in a patient’s VTE risk level is credited with 20% of failures with traditional methods. Additionally, physician-focused VTE programs that are overly complicated may be bypassed.3
The inpatient pharmacist reported that the new process was easily incorporated into daily workflow, with an added benefit of providing a CPRS note for encounter capture and documenting interventions in PhARMD Tool. Feedback from the medical service was that the secondary assessment was helpful in catching overlooked or forgotten pharmacologic orders.
References:
1. Office of the Surgeon General and National
Heart, Lung, and Blood Institute (US). The
Surgeon General’s call to action to prevent deep
vein thrombosis and pulmonary embolism.
Rockville, MD: Office of the Surgeon General
(US);2008.
2. Geerts WH, Pineo GF, Heit JA, et al. Prevention
of venous thromboembolism: the seventh
ACCP Conference on antithrombotic and thrombolytic
therapy. CHEST 2004;126:338s-400s.
3. Maynard G. Preventing hospital-associated
venous thromboembolism: a guide for effective
quality improvement, 2nd ed. Rockville, MD:
Agency for Healthcare Research and Quality; August 2016. AHRQ Publication No. 16-0001-EF.



















