VHA National Center for Patient Safety
Standardizing timeouts at the Phoenix VA
Chief Residents in Quality and Patient Safety teach a quality, process improvement and patient safety curriculum to residents.
The Phoenix VA Health Care System (PVAHCS) has a dedicated inpatient and outpatient Chief Resident in Quality and Patient Safety (CRQS). The chief residents lead a local three-legged curriculum teaching concepts in quality improvement and patient safety to internal medicine residents at the University of Arizona College of Medicine, Banner University Medical Center and PVAHCS.
The three-legged curriculum includes:
• Residents and medical students on VA inpatient rotations are taught about adverse events and near-misses during weekly Electronic Patient Event Reporting (EPER) “happy hours.”These sessions promote electronic patient event reporting and related resident-driven projects.
• The Patient Safety Consult Service (PSCS) consists of senior residents spending a month investigating adverse events and/ or close calls. Stakeholders from various departments meet to discuss causal analysis based on the residents’ Gemba walk and fshbone diagram, and propose plausible system-level interventions to prevent recurrence of the patient safety event.
• The Patient Safety Conference (PSC) is a monthly training event open to all facility staff.
At the PSC, each chief resident leads a one-hour interactive session to address a particular patient safety event. PSCS and PSC involve inter-professional discussions among various departments, including internal medicine residents, nurses, pharmacists, laboratory technicians, radiologists, informatics specialists, medicine subspecialties, VA leadership and faculty.
Through the PSCS, second-year resident Dr. Emma Simpson investigated a patient event involving a wrong-site thoracentesis and identifed the lack of standardized approaches to resident procedures and the importance of timeouts. The Joint Commission states that pre-procedure timeouts immediately prior to the start of invasive procedures reduce wrong site procedures.1
Despite evidence and guidelines to support the use of medical timeouts before invasive procedures, utilization of timeouts among local internal medicine residents is low. Through Dr. Simpson’s survey of 42 internal medicine residents and fellows, only 19 percent (n = 8/42) reported consistently performing pre-procedure timeouts. Common reasons for not performing a timeout were: 1) forgetting, 2) not knowing it was required prior to procedures, and 3) poor understanding of how to perform a timeout.
Based on the survey results, Dr. Simpson and CRQS Dr. Marnonette Marallag collaborated during the November PSC to improve awareness and standardized utilization of medical timeouts for resident procedures.
After attending Dr. Douglas Paull’s simulation module at the CRQS Bootcamp in September 2017, Dr. Marallag used a similar approach to highlight the importance of performing pre-procedure timeouts:
• A conference was conferred including an audience of residents, medical students, faculty and nurses. Inter-professional teams of six were tasked to perform a thoracentesis on a simulation mannequin. However, the patient information given to teams was mismatched. Consequently, nine of 10 teams performed incorrect procedures on the wrong patient because they did not identify the correct patient by name. The audience’s disappointment in their performance underscored the value of this PSC topic.
• As part of the intervention, groups were then introduced to the concept of checklists and their role in the design of pre-procedure timeouts.
• The audience applied the concept of 5S as a workplace tool for organization (i.e., sort, set in order, shine, standardize, and sustain).
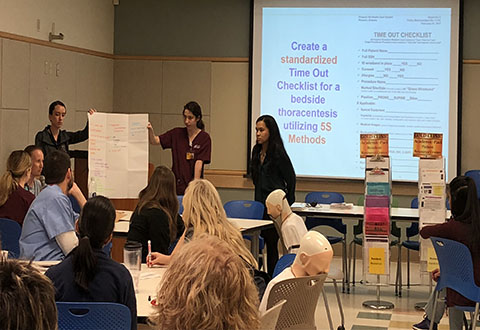
• Each group created a checklist using 5S methods and presented to the larger group.
In summary, the audience reported a greater understanding of the importance of timeouts. A combination of the diferent checklist designs will be applied at the annual internal medicine intern simulation workshop this spring.
For more information on the PVAHCS CRQS curriculum, please contact Dr. Marnonette Marallag at 602-277-5551, ext. 6404.
References:
1. The Joint Commission. (2018). 2018 National Patient Safety Goals. Re¬trieved from https://www.jointcommission.org/standards_information/npsgs.aspx
Article Authors:
Marnonette Marallag, M.D., chief resident in quality and patient safety; Adebisi Alli, D.O., director, quality improvement and patient safety education program, Phoenix VA Health Care System



















